Breast cancer is one of the most common types of cancer in women. Every year, approximately 1,000,00 women in India are diagnosed with breast cancer. Although the disease is widespread, many women are unaware of it until it is too late.
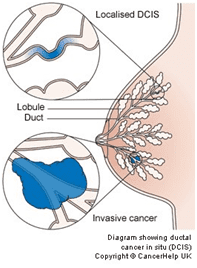
Breast cancer develops in the cells of the breast. It usually starts in the breast lobules or ducts.
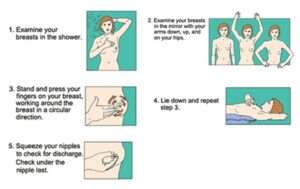
Because breast cancer often shows symptoms, it is critical to self-examine your body and observe any unusual indicators. Something other than cancer could be causing your symptoms. Hence, the only way to be sure is to visit your doctor.
At MACS Clinic, Dr. Sandeep Nayak, with his well-trained team, offers advanced and customized breast cancer treatment in Bangalore, India.
MACS Clinic is regarded as one of the best cancer hospital in Bangalore because we are committed to advancing the diagnosis and treatment of a wide range of malignancies, including breast cancer.
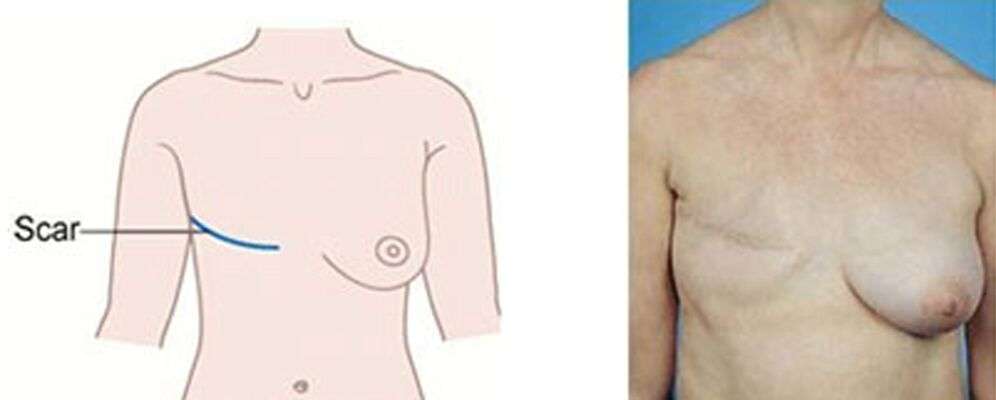
Our clinic is equipped with minimally-invasive surgical techniques and single-day breast cancer radiation therapies like IORT. These methods help the patients recover quickly and offer long-term results.
This article can help if you want to learn more about breast cancer symptoms, diagnosis, and treatments. Continue scrolling to know more.